OXIGEN salud
Infant apnoea monitoring
OXIGEN salud
Infant apnoea monitoring
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of a young baby caused by a cardiac arrest.
It is one of the leading causes of death among babies aged between one month and one year in Spain. In most cases, it takes place between the ages of two and four months, and 90 % of deaths due to this syndrome occur before the age of six months. Beyond this age, the risk decreases.
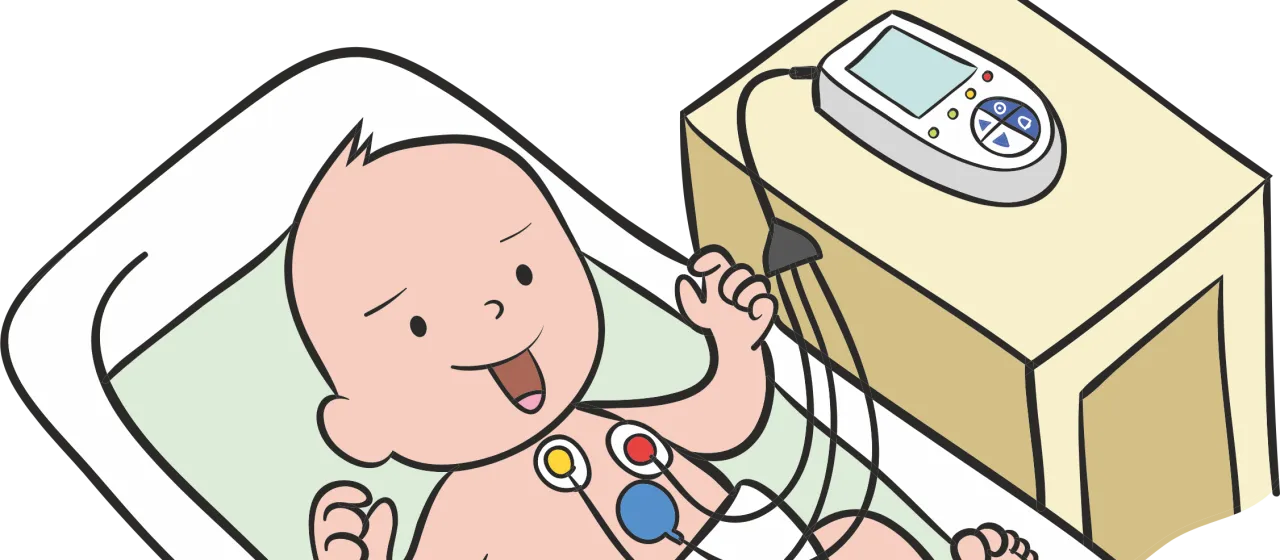
Home apnoea monitoring is used as a method to prevent sudden infant death syndrome (SIDS). Monitors constantly check the infant’s breathing and heart rate, and an alarm goes off if there is any deviation from the defined parameters.
This alarm sound acts as a warning of the occurrence of apnoeas.
This monitoring can be carried out by a small, portable, easy-to-use device. It monitors the infant through two channels, which check their chest movements when inhaling and exhaling and measure their heart rate.
The monitor warns of any breathing cessation (apnoea) or drop in heart rate (bradycardia) through an alarm sound and light.
This device makes it possible to act in time in a situation like those described above, through stimulation or resuscitation if required, though in most cases, the sound of the alarm stimulates the infant and they start to breathe again on their own.
Infant apnoea monitors are equipped with the following alarms:
The care team of OXIGEN salud will install the best portable monitors in the home for infants at risk of SIDS. The baby’s carers will be thoroughly educated on how to use the apnoea monitor. In addition, should there be any queries, the company offers a 24/7 helpline.

Respond as quickly as possible (ideally within 10 seconds). Do not panic and try to stay calm.

If the alarm is a continuous sound, it means there is a problem with the monitor (a loose connection or low battery).
If the alarm is an intermittent sound, it means there is a problem with the baby (an event). The alarm may stop if the event is corrected on its own (tachycardia, bradycardia, low blood oxygen level, apnoea, etc.).

First, check the baby. Ignore the monitor until you are sure the baby is fine.

Check that the baby has not changed colours. Lips and nails are the best places to check the baby’s colour.

Check the baby’s breathing. The baby’s nostrils and abdomen are the best places to check breathing.
If the baby’s breathing and colour are normal, check the electrodes, lead wires and patient cable to find out why the alarm has sounded.

If the baby is not breathing, commence gentle stimulation, and if there is no response, start more vigorous stimulation. If the baby is still not breathing, start CPR and call an ambulance.
If a bag valve mask has been prescribed, it must be used in accordance with the clinical team’s instructions.
Apnoea monitor troubleshooting
| Problem | Cause | Solution |
|---|---|---|
| The apnoea alarm has sounded but the baby is breathing (no colour change). | The belt or electrode is loose. | Check the belt is snug against the chest. |
| The baby’s breathing is shallow. | Make sure the electrodes are placed under the baby’s arms, one on the left side, and one on the right. | |
| The electrodes are dry. | Replace the electrodes with new ones. | |
| Slow heart rate (no colour change). | The belt or electrode is loose. | Check the belt is snug against the chest. |
| The electrodes are dirty. | Replace the electrodes. | |
| There is lotion, oil or baby powder under the electrodes. | Remove any lotion, oil or baby powder from the baby’s skin. | |
| Inappropriate placement for the baby’s age. | Contact a medical professional. | |
| The electrodes are dry. | Replace the electrodes with new ones. | |
| Contact alarms. | The belt or electrode is loose. | Check the belt is snug against the chest. |
| Disconnected. | Check and adjust every connection. | |
| The lead wires are broken. | Replace the lead wires with new ones. | |
| The electrodes are worn. | Replace the electrodes with new ones. |
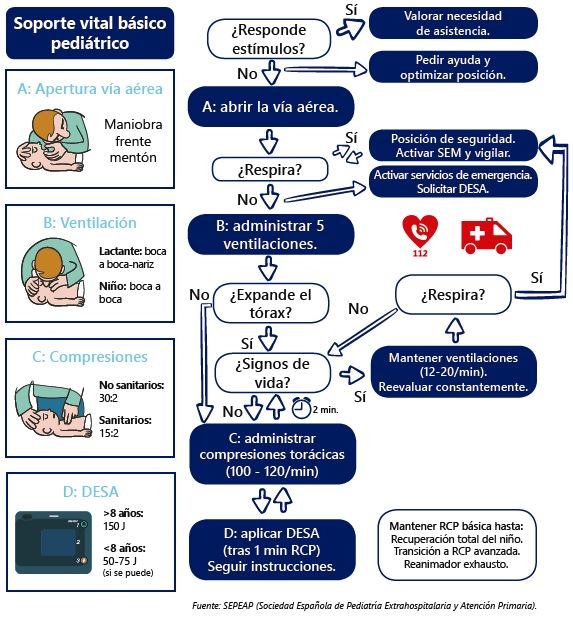
Give cycles of:

30 chest compressions, at a rate of 100 per minute, pushing down 4 cm on the breastbone with 2 or 3 fingers.

2 breaths lasting one second each, using the normal volume of the resuscitator (bag valve mask).
Always begin with the insufflation. Repeat the cycle without interruptions until the baby has fully recovered or until the emergency medical services begin their care.
If the infant is not moving or breathing, call the emergency services number (112).
Some recommendations may help to reduce the risk of SIDS:*
*Data from the NICHD (National Institute of Child Health and Human Development).
Shall we call you?